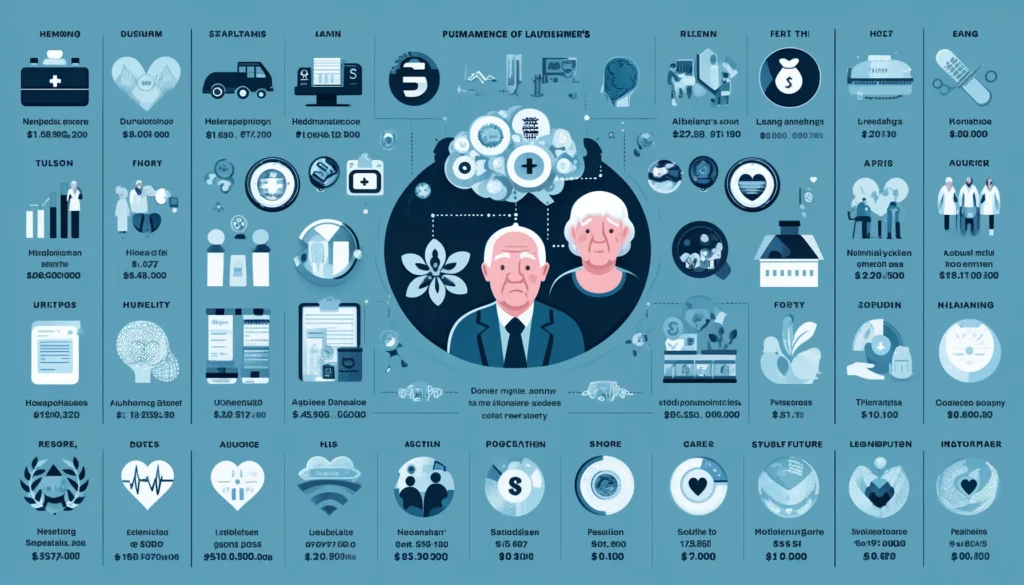
As western societies experience a rapid increase in the size of their aging population, the medical community and pharmaceutical industry are showing heightened interest in diseases prevalent among the elderly. By far the most devastating is Alzheimer s disease, affecting about half of all people over 85. Today, in the U.S. alone, 2.3 million elderly people have Alzheimer s disease and it is predicted that by the middle of next century, about 9 million Americans will have this disease.
The importance of an effective form of treatment is underscored by the true costs neurodegenerative disorders pose to society. It is estimated that the minimal annual costs of Alzheimer s disease is 67 billion dollars in the U.S. and 65 billion Deutsche Marks in Germany. Any treatment that can reduce the rapidly growing financial burden of neurodegenerative disorders and assist the elderly in maintaining independent living arrangements will be a major revenue producer for its developers and distributors.
During the 1990 s, major progress has been made in understanding neurodegenerative diseases, both at the clinical and scientific levels. Advances in understanding pathophysiologic mechanisms have resulted in a wide array of novel treatment approaches. There is now real potential to develop therapies which will slow and possibly stop many of these conditions.
Current research on the mechanisms underlying neurodegenerative diseases focus on:
-therapies based on common or specific disease mechanisms
-future multi-drug or “drug-cocktail” therapies
-patient-specific therapies using pharmacogenomic technologies
Improvement of disease diagnosis and patient identification prior to onset of disease through genetic screening and other technologies. Projection of market trends for neurodegenerative diseases.
Functional Therapeutics in Neurodegenerative Disease
Genetic, toxic, nutritional, traumatic, and lifestyle models have been proposed as playing major roles in the etiology of various neurodegenerative diseases. A model whereby genetically predisposed individuals manifesting demonstrable hepatic detoxification flaws enhancing the neuro-toxic effects of xenobiotics leading to neuronal mitochondrial failure unifies these seemingly disparate theories into an integrated model of neurodegenerative diseases.
The model is an integrated model of neurodegeneration coupling genetics, environment, nutrition, lifestyle, and infection. The theme is that develops is that many exposures can initiate an upregulation of the immune system, which in response releases the inflammatory cytokines. These in turn upregulate the expression of the immune inducible form of nitric oxide synthase. The increased production of nitric oxide in the microglia triggers the depletion of neuronal ATP which in turn increases the activity of xanthine oxidase. This enzyme converts purines to uric acid in the neuron with the production of the reactive oxygen species, superoxide. Superoxide then reacts with nitric oxide to yield peroxynitrite, which results in death of the cell.
Many agents can trigger this cascade in genetically susceptible individuals including bacterial lipopolysaccharides from enteric bacteria, toxic metals and pesticides, food and environmental antigens, stress responses mediated through the pituitary-thyroid-adrenal axis, and chronic infection.
Recently it has been shown that individuals who die of Alzheimer’s disease have a very high gene penetration of apo E4 and a chronic infection with herpes simplex Type 1 (cold sores). Only when both genetic factor apoE4, and the chronic infection are present simultaneously does Alzheimer’s disease result.
Genetic impairment in detoxification ability may also render individuals more susceptible to neurotoxic effects of xenobiotics. The field of pharmacogenics has recently emerged as a discipline of science and medicine focused upon better understanding of how to assess individual detoxification ability. It has been recently reported that older-age individuals who have reduced detoxification ability may be at risk to Parkinsonism symptoms from the use of the drug metaclopramide. Defects in sulfoxidation and Phase II glucuronidation and glutathione conjugation have all been identified as risks to neurodegenerative disease.
The theory helps us to understand better how to ask the right questions concerning the early-stage development of neurodegeneration and provides clues as to its remediation from the answers to these questions.
As it has observed, with many of the neurodegenerative diseases, “the brain is on fire” due to the uncoupling of neuronal mitochondrial function and the release of oxidants. Shifts to anaerobic metabolism often occur with accumulation of cis-aconitate, succinate, and lactate in biological fluids. It is interesting that this situation is observed not only in neurodegenerative diseases, but also with less severity in chronic fatigue syndrome, fibromyalgia, multichemical sensitivity, and individuals with Gulf War Syndrome.

Mitochondrial Dysfunction
The direct clinical consequences of mitochondrial dysfunction in specific diseases have long been appreciated. The clinical manifestation of specific types of mitochondrial pathology are well understood in such syndromes as Kearn-Sayre syndrome (KSS), Leber’s hereditary optic neuropathy (LHON), mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes (MELAS), chronic progressive external ophthalmoplegia (CPEO), Luft’s disease, and others. In these diseases, specific mitochondrial DNA abnormalities and consequent abnormalities of the mitochondrial respiratory chain activity have been well delineated. It is now recognized, however, that acquired mitochondrial DNA abnormalities can also set the stage for significant clinical manifestations. Oxidative damage to mitochondrial DNA has been estimated to be 10-fold higher than damage to nuclear DNA. It has been estimated that mitochondrial DNA mutation rate may be 17 times higher compared to nuclear DNA. These findings are not surprising in that mitochondrial DNA is located in close proximity to the inner mitochondrial membrane which is the site of greatest cellular production of reactive oxygen species (ROS). Further, unlike nuclear DNA, mitochondrial DNA lack significant DNA repair mechanisms.3
It is now known that several important neurodegenerative conditions are characterized by defects of mitochondrial function. In Parkinson’s disease, it has been estimated that there is a 35% deficiency of complex I in the substantia nigra. Deficiencies of cytochrome oxidase (complex IV) activity in the cerebral cortex as well as platelets of Alzheimer’s disease have been reported.
The importance of decreased efficiency of mitochondrial oxidative phosphorylation activity is multi-factorial. Perhaps the most important consequence of inefficient energy production is a change in the neuronal transmembrane potential. Under normal conditions, with adequate mitochondrial energy production, a normal trans-membrane potential exists. The transmembrane potential has a profound effect on the activity of a specific receptor for the excitatory neurotransmitter glutamate. This receptor (NMDA receptor) under normal conditions of transmembrane electrochemical gradient (normal mitochondrial ATP production) is functionally blocked by magnesium ion. When mitochondrial oxidative phosphorylation activity becomes depressed, alterations in the transmembrane potential relieve the magnesium block of the NMDA receptor which, when stimulated by the excitatory neurotransmitter glutamate, causes influx of calcium into the cytosol.
It is the influx of calcium into the cell which plays a pivotal role in the cascade of events leading to neuronal destruction including activation of nitric oxide synthase, increased mitochondrial free-radical production, and activation of proteases and lipases.
It is interesting to note that in Parkinson’s disease, Huntington’s disease, and Alzheimer’s disease, mitochondrial dysfunction leading to excessive free-radical production and oxidative tissue damage seems to be confined to the brain despite the fact that the underlying mitochondrial abnormality is systemic. Indeed, mitochondrial defects in platelets in Parkinson’s disease (50% deficiency in complex I activity) have been well described. This may be explained by the unique susceptibility of the brain to mitochondrial dysfunction and resultant excessive free-radical production since the brain uses approximately 20% of the total O2 consumption (while representing only 1/50th of the body weight). Thus, being so highly metabolic, brain tissue generates more oxyradicals. Second, neurons are post-mitotic. This allows accumulation of oxidatively damaged DNA, proteins, and lipids compared to cells which retain the property to undergo mitosis. Third, compared to other highly metabolic tissues, the brain has relatively low levels of protectant antioxidant enzymes and small-molecule antioxidants.
It has long been known that there is a significant relationship between previous xenobiotic exposure and the risk of various neurodegenerative diseases including Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis. As reported by Semchuk in 1992, “Consistently having a history of occupational herbicide use resulted in a significant increased Parkinson’s disease risk of about three fold”.
If indeed mitochondrial dysfunction plays an important role in the pathogenesis of neurodegenerative diseases and the various studies indicating increased risk with xenobiotic exposure are valid, what mechanism could relate these two concepts? The answer to this question may have been provided in a report by Davis et al. in 1979. This report described the production of a Parkinsonian syndrome in humans exposed to MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyradine), an analog of Meperidine. It was subsequently found that MPTP administered to various animals, predominantly primates, would likewise produce a syndrome mimicking human Parkinson’s disease. Further, animals treated in this manner were found to be responsive to typical anti-Parkinsonian medications. The discovery of MPTP provided valuable information, which has a direct bearing on the understanding of the etiology of Parkinson’s disease. First, it has been discovered that MPTP is a specific direct inhibitor of complex I of the electron transport chain.10 Inhibition of complex I causes depletion of ATP production, altering the neuronal trans-membrane gradient rendering the NMDA receptor more receptive to glutamate. The resulting influx of calcium enhances reactive oxygen species generation which further damages mitochondrial activity in a self-propagating feed-forward cycle, ultimately leading to cell death. The importance of NMDA receptor sensitivity as a link in this destructive chain is exemplified by the work of Tursky who demonstrated that blocking the NMDA receptor with specific antagonists would prevent damage to the substantia nigra in experimental animals exposed to MPTP. Further, it appears that nitric oxide plays a pivotal role in the toxicity to substantia nigra neurons induced by MPTP. Mice pre-treated with 7-nitroindazole, a nitric oxide synthase inhibitor, demonstrate a dose-dependent protection against MPTP substantia nigra damage. This implies that nitric oxide formation also plays an important role with respect to free-radical neuronal damage induced by mitochondrial energy production dysfunction. Clarification of the mechanism of neuronal injury whereby MPTP is metabolized to reactive MPP+, which is then selectively transported across the neuronal membrane by specific dopamine transporters leading to mitochondrial damage, has encouraged researchers to identify other exogenous or endogenous chemicals which may act in a similar fashion.
Recently, N-methyl-(R)-salsolinol is identified as a possible endogenous MPTP-like neuro-toxin. The possibility that xenobiotics may act in a fashion similar to MPTP, coupled with the obvious link of Parkinson’s disease risk with pesticide exposure, has encouraged research specifically focused on the role of xenobiotics as toxic agents with respect to mitochondrial function. In a study reported by Flemming et al., Dieldrin, a lipid-soluble long-lasting mitochondrial toxic pesticide, was found in six of twenty brains of Parkinson’s patients and in none of controls.
But what appears as perhaps an obvious question with respect to the increased risk of Parkinson’s in individuals exposed to pesticides is why some of those exposed will manifest the disease while most will not. Could some individuals manifest dysfunction of xenobiotic metabolism to the extent that toxic metabolites are not cleared appropriately and thus remain within the body, ultimately inflicting damage on delicate neuronal homeostatic mechanisms? The answer to this question has perhaps best been answered by Steventon and others who have demonstrated significant abnormalities of xenobiotic metabolism in Alzheimer’s disease, Parkinson’s disease, motor neuron disease, and even rheumatoid arthritis. The specific abnormalities of detoxification described by these authors involve decreased activity of phase II sulfation. Phase I abnormalities including the P450 enzymes IID6 and cysteine dioxygenase have also been described. Identification of “at risk” individuals, i.e., those individuals with inherited hepatic detoxification flaws, may allow the development of preventive strategies to reduce the likelihood of disease manifestation. Specific evaluation of hepatic detoxification pathways is now widely available.
The NMDA Receptor
In recognizing the importance of the NMDA receptor in the cascade ultimately leading to neuronal death, various schemes have been proposed to block the glutamate stimulation of this receptor. It has long been recognized that patients treated with Amantadine for Parkinson’s disease survived longer compared to those who did not receive this medication. The specific mechanism by which Amantadine may be helpful in this regard may stem from its “neuro-protective” effect mediated through the antagonism of the NMDA receptor. Inhibiting glutamate stimulation of the NMDA receptor is the proposed mechanism by which gabapentin and riluzole have purported efficacy in motor neuron disease. The use of branched chain amino acids (L-leucine, L-isoleucine, and L-valine) in amyotrophic lateral sclerosis, although not having been shown to be significantly effective, was proposed as this group of amino acids is known to inhibit glutamate production. Further, excessive glutamate as a consequence of deficient clearance from the synaptic cleft may represent a specific mechanism for excessive NMDA receptor stimulation in amyotrophic lateral sclerosis.
Nitric Oxide
As described above, nitric oxide (NO) seems to play a pivotal role in the cascade of events leading to neuronal death following glutamate stimulation of the NMDA receptor. Nitric oxide is formed when L-arginine is oxidized to citrulline by the action of the enzyme nitric oxide synthase. Although nitric oxide itself is a free radical due to its unpaired electron, it is not felt to participate in any significantly damaging chemical reactions in and of itself. However, when reacting with superoxide anion, the extremely reactant and potent oxidant peroxynitrite (ONOO) is formed. This reaction is approximately three times faster than the reaction dismutating superoxide to form hydrogen peroxide catalyzed by superoxide dismutase (SOD). Peroxynitrite has been implicated in a variety of damaging intra-neuronal events including DNA strand breaks, DNA deamination, nitration of proteins including superoxide dismutase, damage to mitochondrial complex I, complex II, and mitochondrial aconitase. In addition, nitric oxide itself also specifically damages mitochondrial complex I.
Thus, nitric oxide physiology has been a central focus of research in the neurodegenerative diseases. Inhibiting its synthesis may provide an avenue for reducing the neuro-destructive capabilities of extrinsic toxins which may have implications in the neurodegenerative disorders, if in fact extrinsic toxins (or even endogenously produced toxins) participate in chronic expression of nitric oxide synthase. The role of nitric oxide in the pathogenesis of Parkinson’s disease is exciting and remains the focus of vigorous research. Hantraye and associates in Orsay, France published research in 1996 demonstrating that pre-treatment of baboons with the nitric oxide synthase inhibitor 7-nitroindazole (7-NI) completely prevented the induction of Parkinsonism in baboons exposed to MPTP. These researchers demonstrated that inhibiting nitric oxide synthase “protected against profound striatal dopamine depletion and loss of tyrosine hydroxylase-positive neurons in the substantia nigra” and “protected against MPTP-induced motor and frontal-type cognitive deficits.”
Elevated levels of nitric oxide synthase have been found in the brains of patients with multiple sclerosis. Bagasra and colleagues at Thomas Jefferson University demonstrated elevated levels of nitric oxide synthase messenger RNA in 100% of the CNS tissues from seven multiple sclerosis patients, but in none of three normal brains. The authors conclude, “These results demonstrate that NOS, one of the enzymes responsible for the production of nitric oxide, is expressed at significant levels in the brains of patients with MS and may contribute to the pathology associated with the disease.”
Nitric oxide may also play an important role in the pathogenesis of Alzheimer’s disease. Beta-amyloid plaques are a characteristic histopathological finding in Alzheimer’s disease. When cultured rat microglia are exposed to beta-amyloid, there is a prominent microglial release of nitric oxide especially in the presence of gamma- interferon. In cortical neuronal cultures, treatment with nitric oxide synthase inhibitors provides neuro-protection against toxicity elicited by human beta-amyloid.
The role of nitric oxide in mediating neuronal damage in cerebral ischemia is also the subject of intense research. Again, the operative model recognizes excessive glutamate stimulation of the NMDA receptor in cerebral ischemia with elevation of intracellular calcium and induction of nitric oxide synthase raising intra-neuronal nitric oxide. In addition, elevated cytosolic calcium converts the enzyme xanthine dehydrogenase to xanthine oxidase which results in excessive superoxide anion formation, thus setting the stage for the production of the highly reactive peroxy-nitrite radical (ONOO-) via the mechanism described above. Transgenic mice over-expressing SOD with resultant decreased superoxide formation are protected against focal ischemia, as are mice which genetically lack nitric oxide synthase.
Because of the wide-ranging implications of nitric oxide chemistry in both acute and chronic neuro-destructive entities, selected inhibition of nitric oxide synthase has become the focus of extensive pharmaceutical research. Specific attempts to inhibit nitric oxide synthase include the use of arginine analogues, which compete with L-arginine for catalytic binding sites on nitric oxide synthase. Arginine analogues, however, are associated with profound cerebral vaso-constriction and thus may result in worsening perfusion.
Nutritional approaches focusing on increased dietary citrulline may offer an alternative approach to reducing nitric oxide formation. As noted by Larrick, “Although citrulline is not one of the amino acid building blocks of protein, large quantities of free citrulline do occur in some foods such as watermelon, Citrullus vulgaris, which contains 100 mg/100 grams.”
Substituted guanidoamines may demonstrate therapeutic promise through the mechanism of inhibition of nitric oxide synthase, especially in multiple sclerosis. In auto-immune encephalomyelitis in mice (an animal model for multiple sclerosis), aminoguanidine, an inhibitor of nitric oxide synthase, when administered to mice sensitized to develop experimental auto-immune encephalomyelitis, specifically inhibited disease expression in a dose-related manner.
Functional Intervention
The energy-linked excitotoxic model described above reveals multiple targets of susceptibility whereby compromised function can begin a progressive, feed-forward and thus self-perpetuating cascade ultimately culminating in neuronal death. These include excessive glutamate leading to excessive NMDA receptor stimulation (as noted in cerebral ischemia and amyotrophic lateral sclerosis); enhanced NMDA receptor sensitivity to glutamate as a consequence of altered electro-chemical gradient due to decreased mitochondrial ATP production (as noted in idiopathic Parkinson’s disease, MPTP-induced Parkinsonism, Huntington’s chorea, Alzheimer’s disease, and various inherited mitochondropathies); formation of NMDA receptor antibodies allowing persistent cellular inflow of calcium (noted in amyotrophic lateral sclerosis); enhanced nitric oxide production (as noted in Parkinson’s disease, Alzheimer’s disease, animal models, multiple sclerosis animal models, and ischemic stroke); deficiencies of small molecule antioxidants and antioxidant enzymes (Huntington’s chorea, Alzheimer’s disease, amyotrophic lateral sclerosis, and Parkinson’s disease); and deficiencies of xenobiotic metabolism allowing accumulation of neuro-toxic intermediates (amyotrophic lateral sclerosis, Alzheimer’s disease, and Parkinson’s disease).
Inhibition of Glutamate Release/NMDA Stimulation
A number of protective agents are thought to act by inhibiting either the release of glutamate or the subsequent stimulation of the NMDA receptor. These include the anti-convulsants gabapentin, lamotrigene, diphenylhydantoin, carbanazepine, and riluzole, a pharmaceutical agent developed for the treatment of amyotrophic lateral sclerosis. Huperzine A, an ancient Chinese herbal medicine (Qian Ceng Tan), was recently described in the Journal of the American Medical Association as a possible new therapy for Alzheimer’s disease. In addition to having acetylcholinesterase inhibition activity, Huperzine A specifically inhibits glutamate stimulation of the NMDA receptor.
Mitochondrial Function
One of the most promising agents for up-regulation of mitochondrial function is Coenzyme Q-10. Coenzyme Q-10, in addition to having free-radical scavenging properties, is known to play a pivotal role in transporting electrons in the mitochondria for ATP production. The usefulness of Coenzyme Q-10 in specific mitochondrial myopathies has been well described. Bresolin and co-workers in Milano, Italy have described enhanced mitochondrial activity as evidenced by reduction of serum lactate and pyruvate following standard muscle exercise with generally improved neurologic functions in Kearns Sayre syndrome and chronic progressive external ophthalmoplegia. Idebenone, a Coenzyme Q-10 derivative with increased blood-brain barrier penetration, produced enhanced cerebral metabolism in a 36-year-old man with MELAS (mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes) during a five-month treatment protocol providing Idebenone up to 270 mg per day. Cerebral metabolism in this study was followed with PET (positron emission tomography) studies.
Finally, preliminary studies have demonstrated lowering of cerebral lactate levels in vivo in Huntington’s disease in a patient receiving Coenzyme Q-10 310 mg per day. There was an average of 29% decrease in lactate levels following treatment as demonstrated by magnetic resonance spectroscopy.
Phosphatidylserine enhances both neuronal and mitochondrial stability and activity and reduces mitochondrial free-radical production. Researchers at Stanford University School of Medicine evaluated a group of 149 patients meeting criteria for “age-associated memory impairment” over a period of twelve weeks with either phosphatidylserine (100 mg t.i.d.) or placebo. Actual improvement in the treated group on psychometric testing related to learning and memory was seen in a majority of patients, specifically those who had scored above the range of cognitive performance associated with dementing disorders such as Alzheimer’s disease, but who were performing in the low normal range for persons of the same age. As the authors reported, “Results of this study suggest that phosphatidylserine may be a promising compound for the treatment of memory deficits that frequently develop in the later decades of adulthood. Effects were present on a number of outcome variables related to such important tasks of daily life as learning and recalling names, faces, and numbers. Drug effects may also generalize to other difficult tasks involving learning, memory, and concentration since improvement was also present on a standard neuro-psychological test that measures the ability to remember details of a story after it is read. This finding may be related to the common complaint in later adulthood of difficulty in remembering what one just read in a newspaper, book, or magazine article.” Similar results have been noted in other studies.
Monoamine oxidase type B (MAO-B) catalyzes the oxidation of dopamine to dihydroxyphenylacetaldehyde with formation of hydrogen peroxide. In the absence of adequate glutathione peroxidase (well described in Parkinson’s disease), excessive hydrogen peroxide is available to participate in the Fenton reaction whereby hydrogen peroxide combines with ferrous iron forming ferric iron and the highly reactive hydroxyl radical. Thus, inhibition of MAO-B may offer therapeutic benefit in Parkinson’s disease and in other neurodegenerative conditions characterized by free-radical production as a consequence of oxidation of cerebral catecholamines. Selegeline, a potent inhibitor of MAO-B, having long been demonstrated to delay the need for dopamine-replacement therapy in Parkinson’s disease, is now being evaluated for its ability to improve cognitive defects associated with Alzheimer’s disease.38 Interestingly, it has been demonstrated that extracts of Ginkgo biloba leaf also have a profound inhibitory influence on MAO-B. In addition, Ginkgo biloba is known to be involved in such diverse processes as homeostasis of inflammation, reduction of oxidative stress, membrane protection, and neuro-transmission modulation. Le Bars and co-workers, in research recently published in the Journal of the American Medical Association, evaluated 202 patients suffering from Alzheimer’s disease or multi-infarct dementia over a 52-week period of time. These subjects received either an extract of Ginkgo biloba or placebo. In the treatment group a substantial number of patients either stabilized or actually demonstrated improvement in cognitive performance as measured by psychometric testing, and this was of sufficient magnitude that it was frequently recognized by the care-giver.
Increased intra-cellular calcium is known to enhance the conversion of the enzyme xanthine dehydrogenase (which metabolizes xanthine to uric acid plus NADH) to xanthine oxidase (converts xanthine to uric acid plus superoxide radical). This provides another mechanism whereby increased cytosolic calcium enhances the free-radical load. Unpublished research by Dr. Stanley Appel is evaluating the efficacy of allopurinol (a potent inhibitor of xanthine dehydrogenase and xanthine oxidase) in amyotrophic lateral sclerosis. Clearly, the enzymatic shift favoring xanthine oxidase with its resultant increase in superoxide formation has implications in many other neurodegenerative entities. Since allopurinol inhibits both xanthine dehydrogenase and xanthine oxidase, overall production of uric acid is decreased. Uric acid may have antioxidant properties, thus selective inhibition of xanthine oxidase would be more ideal. Sheu and co-workers at Tai Pei Medical College have demonstrated the specific inhibitory effect of silymarin on xanthine oxidase.
As described above, the role of nitric oxide in acute and chronic neurological illnesses is multi-factorial. Dietary inhibition of nitric oxide formation by citrulline was described above. Kong, and co-workers at the National Institute of Environmental Health Sciences have demonstrated that glial cell cultures stimulated to produce nitric oxide by a combination of lipopolysaccharide and interferon-gamma are significantly inhibited with respect to nitric oxide production when treated with genistein.
Acetyl-L-carnitine has been demonstrated to specifically increase cellular ATP production. It was shown to prevent MPTP-induced neuronal injury in rats. Further, Acetyl-L-carnitine reduces production of mitochondrial free-radicals, helps maintain transmembrane mitochondrial potential, and enhances NAD/NADH electron transfer. Thal and colleagues at the University of California San Diego evaluated the efficacy of Acetyl-L-carnitine, 1 gram t.i.d. for twelve months in a multi-center, placebo-controlled study of 431 patients with Alzheimer’s disease, 83% of whom completed the one year study. Their results demonstrated “…a trend for early-onset patients on Acetyl-L-carnitine to decline more slowly than early-onset Alzheimer’s disease patients on placebo.”
Alpha lipoic acid is emerging as one of the most promising agents for neuro-protection in neurodegenerative diseases. This potent antioxidant demonstrates excellent blood-brain barrier penetration. It acts as a metal chelator for ferrous iron, copper, and cadmium, and also participates in the regeneration of endogenous antioxidants including vitamins E, C, and glutathione. Although no large clinical evaluation of the usefulness of alpha lipoic acid in neurodegenerative diseases has as yet been published, an excellent review in a paper entitled “Neuro-protection by the metabolic antioxidant alpha lipoic acid” by Packer and co-workers in Frankfort, Germany provides enough justification for strong consideration of alpha lipoic acid as a neuro-protectant for neurodegenerative conditions.
The lipophilic antioxidant vitamin E is thought to play a major role in defending mitochondria against oxidative stress. Since mitochondrial ATP production is a membrane-bound event, reducing oxidative membrane damage would likely slow the decline of oxidative phosphorylation potential. In a report published in the New England Journal of Medicine, researchers at Columbia University College of Physicians and Surgeons studied 341 patients with Alzheimer’s disease of moderate severity receiving selegeline 10 mg per day, alpha-tocopherol (vitamin E) 2000 i.u. a day, both, or placebo, over a two-year period of time. The results revealed that the primary outcomes of death, institutionalization, loss of the ability to perform basic activities of daily living, or severe dementia were prolonged in the groups receiving selegeline or vitamin E compared to the groups receiving placebo or selegeline and vitamin E.
Melatonin, in addition to having free-radical scavenging properties, has also been demonstrated to increase gene expression for antioxidant enzymes. Kotler has demonstrated increased levels of mRNA for glutathione peroxidase, copper-zinc superoxide dismutase, and manganese superoxide dismutase in melatonin-treated rat brain cortex.51 These properties in addition to the ability of melatonin to readily traverse the blood-brain barrier as well as its lipid and aqueous solubility provide substantiation for consideration of melatonin in neurodegenerative conditions.
Glutathione is an important cerebral mitochondrial antioxidant maintaining both vitamin E and vitamin C in their reduced state and removing potentially damaging peroxides. A profound decrease in brain glutathione has been demonstrated in Parkinson’s disease. Intravenous reduced glutathione has been used as a treatment of early Parkinson’s disease. Sechi administered reduced glutathione 600 mg twice daily for thirty days in an open label study on patients with early Parkinson’s disease. All patients improved “significantly” after glutathione therapy, with a 42% decline in disability. The therapeutic effect lasted for 2-4 months after therapy. They concluded, “Our data indicate that in untreated Parkinson’s disease patients, glutathione has symptomatic efficacy and possibly retards the progression of the disease.”
The nutritional supplement N-acetyl-L-cysteine has been demonstrated to increase intra-cellular cysteine levels, enhancing glutathione production. In addition, glutathione may be enhanced by the use of alpha lipoic acid (see above), L-cysteine, L-methionine, L-glutamine, reducing xenobiotic challenges, reducing drug challenges which induce cytochrome P450 enzymes, complementary antioxidants including vitamins C and E, and silymarin, which acts by increasing glutathione retention. Finally, it is noted that N-acetyl-cysteine may act as a potent antioxidant in that it inhibits the production of nitric oxide. NADH plays a pivotal role in the function of complex I of the respiratory chain. Enzyme function of NADH ubiquinone reductase in the platelets of Parkinson’s disease patients is noted to be 30-60% lower than that of aged match controls. This activity increases following administration of NADH. Birkmayer has demonstrated improvements of short-term memory and other cognitive functions in Parkinson’s patients treated with NADH. He felt that NADH would prove helpful in Parkinson’s disease since NADH stimulates tyrosine hydroxylase, the rate-limiting enzyme for dopamine biosynthesis. Because deficiencies of dopamine and noradrenalin are found in patients with senile dementia of the Alzheimer’s type, he studied the usefulness of NADH in 17 patients suffering from dementia of the Alzheimer’s type in an open label trial. Using the mini-mental status examination, he found that all 17 patients treated with NADH, 5 mg twice a day, improved. Minimum improvement was 6 points with a maximum of 14 and a mean of 8.35 points with therapy ranging from 8 to 12 weeks.
Proteomics
Significant proteomic approaches have been used to study degenerative diseases, including Alzheimer’s disease, and many protein classes from signalling, metabolic, cytoskeleton, chaperone, antioxidant, and proteasome have been shown to be tentatively involved in pathological mechanisms. The aim of this review is to show what has been studied so far in the area using proteomic approaches, describing methodologies used including their potentials and limitations, and finally what still remains to be done.
Bioinformatics and Brain Imaging
Medical imaging and brain research are among the most challenging and fascinating topics of contemporary science. Exciting possibilities exist to improve both the state of the art in medicine and our understanding of the human brain. These opportunities have motivated many researchers to use powerful computational methods to analyze images of brain structure and function, applying them to key questions in medicine and neuroscience. Algorithms can now uncover disease-specific patterns of brain structure and function in whole populations. These tools now chart how the brain grows in childhood, detect abnormalities in disease, and visualize how genes, medication, and demographic factors affect the brain. Image analysis methods can also identify and monitor systematic patterns of altered anatomy in diseases such as Alzheimer’s, tumor growth, epilepsy, and multiple sclerosis, and psychiatric disorders such as schizophrenia, autism, and dyslexia.
Nerve growth factor (NGF), a member of the neurotrophin family, is a homodimer implicated in the differentiation and survival functions of neurons. Nerve growth factor (NGF) is one of a family of neurotrophins that induce the survival and proliferation of neurons. In cell culture NGF induces the formation of neurite projections and in vivo may stimulate the innervation of tissues. NGF plays a role in the repair, regeneration, and protection of neurons, and as such could serve as a therapeutic agent in neurodegenerative conditions such as Alzheimer’s disease. One potential method of NGF application would be through gene therapy or through implantation of cells that have been genetically modified ex vivo. NGF has also been suggested to play a role in other physiological systems and tissues such as the immune system.
NGF has two receptors, TrkA and the p75(NTR). NGF may signal its neuroprotective actions through the tyrosine kinase TrkA receptor and trigger apoptosis in some cells through the p75 receptor. High-affinity binding of NGF requires both TrkA and p75(NTR). Binding of NGF to the TrkA receptor causes activation of the receptor tyrosine kinase and downstream signaling cascades. One of the downstream signaling pathways of NGF activates phospholipase C, releasing DAG and IP3 and activating associated downstream pathways such as protein kinase C. Another NGF-activated pathway is the ras-mediated activation of the map kinase pathway. This pathway is initiated through recruitment and activation of Shc, which leads to ras activation through Grb-2 and Sos-1. The Map kinase cascade includes raf, Mek and Erk. The downstream effectors of the ras pathway include activation of fos and jun to form AP-1, activating genes through this transcription factor. Other transcription factors involved in NGF responses include Egr and CREB. The Egr family of transcription factors as well as the Mek/Erk pathway contribute to NGF-induced neurite formation. The CREB family of transcription factors are involved in NGF-induced survival of sympathetic neurons. Further understanding of NGF signaling may be applied to the modulation of NGF responses in neurodegenerative conditions.It has been shown that Nerve growth factors (NGF, BDNF) enhance axonal regeneration but are not required for survival of adult sensory neurons.
Alzheimer’s disease (AD) is the most common form of dementia in the UK and is the 4th most common cause of death after heart disease, cancer and stroke. The risk of illness in the population varies with age. Less than 1 in 100 people below the age of 65 are affected by AD but this figure increases to almost 1 person in 2 over the age of 90. As the proportion of the UK population living into the high risk age group for AD is increasing, the number of people with AD is expected to substantially increase. Without progress in treatment, this will undoubtedly have an enormous impact on an increasing number of affected individuals, their families and carers, and society as a whole.
Proteomics also has been hailed as the next step in basic science contributing to diagnosis and therapy for neurological disorders (e.g., Creutzfeld-Jakob disease), infectious diseases such as tuberculosis, heart failure, and cancer. Proteomics will no doubt present novel challenges in research, but the purported clinical benefits seem well worth the difficulty. The information yielded by proteomics will not only push the limits of genomics, but also push the frontiers of the current biomedical revolution.
New Medications For Parkinson’s Disease
Dopamine Agonists
The role of dopamine agonists as solely adjunctive medications to levodopa is changing. Recent studies of the new dopamine agonists clearly demonstrate they are effective in reducing the motor symptoms (tremor, rigidity, bradykinesia) of Parkinson’s disease as monotherapy as well as when added to levodopa. Off time decreases by 30% to56%, less on/off fluctuations occur and a recent 5 year study showed a markedly lower incidence of dyskinesia in the patients on monotherapy ropinerole of 5% when compared to the monotherapy levodopa rate of 46%. Similar data has been reported in MPTP-treated monkeys for bromocriptine and ropinerole. There is also evidence that dopamine agonists may be neuroprotective of dopaminergic neurons. Taken together, these findings support the use of dopamine agonists as monotherapy in newly diagnosed, early and mild to moderate Parkinson’s disease and adding levodopa therapy when the patients motor symptoms are not adequately controlled by dopamine agonists alone or intolerable side effects develop.
Four dopamine agonists are available in the United States and include bromocriptine, pergolide, mirapex and ropinerole. The new, second generation agonists, mirapex andropinerole are structurally more similar to the dopamine molecule, lack the ergot structure of the first generation agonists, are potent D-2 agonists similar to pergolide, and have little or no binding to alpha, beta, and serotonin receptors. Despite these differences, no one dopamine agonist has been shown to be superior to another in the treatment of the motor symptoms of Parkinson’s disease. They all may produce similar side effects of nausea/vomiting, light headedness, orthostasis, peripheral edema, sedation and confusion/hallucinations. The ergot agonists have rarely been reported to cause retroperitoneal and pulmonary fibrosis, erythromelalgia and Raynaud’s like syndrome. In the authors experience ropinerole has a lower CNS side effect profile and maybe a more appropriate agonist for an elderly Parkinson’s patient with preexisting confusion or dementia. Recent reports in the literature have implicated sudden sleep attacks in Parkinson’s patients taking mirapex and in only one patient taking ropinerole with some of these attacks occurring while the patient was driving.
COMT Inhibitors
COMT inhibitors act by inhibiting the enzyme catecholamine-o-methyltransferase which is responsible for metabolizing levodopa to 3-O-methyldopa in the peripheral bloodstream. By inhibiting COMT, these drugs result in an increase in the half-life of levodopa and an increase in the bioavailability of levodopa such that a more continuous and greater amount of levodopa crosses the blood brain barrier to act directly on dopaminergic neurons. Tolcapone was released in March of 1998 and Entacapone was released in November of 1999. Both result in a decrease in the “off” time by 1 to 3 hours per day, a decrease in motor fluctuations and allowed for a reduction in the total levodopa daily dose by 10 to 30%. COMT inhibitors are indicated for use as adjunctive therapy to levodopa in Parkinson’s disease patients who experience wearing “off” and motor fluctuations.
Both drugs may cause levodopa side effects of dyskinesias, nausea, confusion and sedation that are easily controlled by lowering the levodopa dose. Non levodopa side effects include diarrhea (3 to 4%) and urine discoloration. Tolcapone results in an increase in liver enzymes in only 1 to 3% of patients. Three cases of fatal liver failure out of 60,000 patient years have been reported with the use of tolcapone and the FDA has mandated that patients on tolcapone have frequent liver function testing. Patients taking tolcapone must have their liver function checked every 2 weeks for the first year, followed by one a month for the next 6 months and then every 2 months there-after. No cases of elevated liver enzymes or hepatotoxicity have been reported with entacapone to date.
Dosing of the COMT inhibitors varies between the two drugs. Tolcapone should be started at 100 mg three times a day separated by 6 to 8 hours and if no significant benefit is noted by 2 to 3 weeks one should either discontinue the drug or consider increasing the dosage to 200 mg t.i.d. If however at the higher dosage no significant clinical improvement is observed the drug should be stopped. Entacapone comes only in 200 mg pills and it is recommended that the patient take one pill each time they take levodopa up to a maximum of 8 total pills per day. As with tolcapone if no clinical benefit is noted one should consider stopping the drug. Due to the relatively little time entacapone has been available it is difficult to comment on it’s true clinical impact on the treatment of Parkinson’s disease. Tolcapone, on the other hand, has been used worldwide for over a year and a half and in the author’s personal experience, it is clearly miraculous in a select group of patients suffering from motor fluctuations. Three patients I personally treated had such severe motor fluctuations that all three were candidates for neurosurgical treatments and all three dramatically improved with the addition of tolcapone such that we were able to lower their levodopa doses and avoid pursuing neurosurgical therapies.
Interventional Neuroradiology is a growing subspecialty that uses techniques to treat vascular problems of the brain and spine. These treatment strategies involve the use of catheters (hollow plastic tubes) to treat the problem from inside the blood vessel, endovascularly.
In the last 15 years, both imaging technology and equipment technology have made great strides, allowing previously untreatable lesions to become treatable. Often these techniques eliminate the need for open surgery. The recovery time for these procedures is very short. Interventional Neuroradiology group has been at the forefront of the development of endovascular therapy to treat a diverse group of diseases including aneurysms, arteriovenous malformations (AVMs), and atherosclerosis.
Over the next several decades, Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, multiple sclerosis, and other neurodegenerative diseases will have an ever increasing impact on our society emotionally, socially, and financially.